Understanding Osteoarthritis:
Symptoms, Diagnosis, and Treatment
Imagine waking up every morning with a stiffness in your knees that makes even walking to the kitchen feel like a chore.
That's the reality for many people living with osteoarthritis. Find out how to manage joint pain and get your life back.
This guide provides a full overview of osteoarthritis, from symptoms to treatment.
Pratik Chapagain, MS, Biomedical Engineer
Dec 11, 2025
Are you experiencing persistent joint pain, stiffness, or that grating feeling when you move? You might be searching for answers to what's causing these sensations. If so, you've come to the right place. While Osteoarthritis (OA) is often dismissed as a simple consequence of aging, modern medicine now recognizes it as a complex disease affecting the entire joint. The good news? We have more tools and knowledge than ever before to manage it effectively.
This guide will provide a comprehensive overview of osteoarthritis, from its causes and symptoms to the full range of treatment options available today.
Table of Contents
What is Osteoarthritis?
Osteoarthritis (OA), also known as degenerative joint disease, is the most common form of arthritis, affecting about 33 million adults in the United States alone. While it's historically been referred to as a "wear and tear" condition often associated with aging, experts now understand that it's a disease of the entire joint, impacting bone, cartilage, ligaments, fat, and the tissues lining the joint. At its core, Osteoarthritis is a degenerative joint disease characterized by the breakdown of cartilage—the firm, slippery tissue that cushions the ends of bones in a joint. As cartilage wears away, the bones can begin to rub against each other, leading to pain, swelling, and stiffness.
While OA is more common in older individuals, it's not simply a natural part of aging. It can also be caused by joint injuries, repetitive stress, and other risk factors like obesity and genetics. The disease often progresses slowly over time, making it crucial to understand the signs and seek treatment early.
OA can affect any joint, but it most commonly develops in the hands, knees, hips, neck (cervical spine), and lower back (lumbar spine). It can be classified into two types:
-
Primary Osteoarthritis: This is the most common form, believed to be caused by the normal wear and tear of using your joints throughout your life. It typically develops slowly.
-
Secondary Osteoarthritis: This type occurs when a specific event, like a joint injury or trauma (such as a torn ACL or meniscus), directly damages a joint enough to cause OA. It can develop much more rapidly, sometimes within just a few years.
What Causes Osteoarthritis?
While once thought to be a simple result of "wear and tear", osteoarthritis (OA) is now understood to be a complex disease with multiple contributing factors. It is a disease of the entire joint, and while the exact trigger for its onset remains under study, researchers have identified several key risk factors that lead to the breakdown of cartilage and the subsequent pain and stiffness.
Understanding the Role of Cartilage
OA is a disease of cartilage degradation. Healthy cartilage is the smooth, slippery tissue that cushions the ends of bones within a joint. When it wears away, bones can rub directly against each other. This friction causes pain, swelling, and a loss of joint function. The breakdown of this critical tissue is not always a linear process. It can be triggered by a combination of mechanical stress and biological factors.
The Key Causes and Risk Factors
A number of factors, both modifiable and non-modifiable, can increase a person's risk of developing osteoarthritis.
-
Age: While not a direct cause, the risk of developing OA increases significantly as you get older. The cumulative stress on joints over a lifetime can lead to a gradual breakdown of cartilage. It's important to remember that OA is not an inevitable part of aging; many people never develop it.
-
Joint Injury or Trauma: A significant injury to a joint can be a direct cause of post-traumatic osteoarthritis. This can happen from a sports injury, car accident, or other trauma that damages the cartilage, ligaments, or surrounding bone. These injuries can alter the mechanics of the joint, leading to a much faster onset of OA, sometimes within just a few years.
-
Repetitive Stress or Overuse: Jobs or sports that require repetitive motions can place constant stress on certain joints, accelerating the wear of joint cartilage.
-
Obesity: Excess body weight is a significant, and modifiable, risk factor for OA, particularly in weight-bearing joints like the knees and hips. The added pressure on the joints accelerates the breakdown of cartilage. Moreover, fat tissue produces proteins that can cause inflammation in and around the joints, contributing to the development of OA.
-
Genetics: A person's genetic makeup can play a role in their likelihood of developing OA, as certain inherited traits can affect the structure of cartilage or the alignment of bones.
-
Bone or Joint Deformities: People born with malformed joints or defective cartilage may be more susceptible to OA. These structural abnormalities can lead to poor joint alignment and an accelerated rate of wear.
-
Gender: Women are more likely than men to develop osteoarthritis, especially after the age of 50. While the exact reasons are still being researched, hormonal changes and bone density differences may be contributing factors.
The Role of Inflammation
Recent research has shown that inflammation is a key component of osteoarthritis. While it was once thought to be a purely mechanical issue, we now know that OA is a disease of the entire joint, including the synovial lining, which can become inflamed. This inflammation contributes to pain and further cartilage degradation, creating a destructive cycle
A Modern Understanding
Our understanding of what causes osteoarthritis has evolved significantly. It's not a simple case of a joint "wearing out" but a complex interplay of a person's biology, lifestyle, and history of injury. By recognizing these contributing factors, we can better manage the disease and focus on strategies for both prevention and effective treatment.
By understanding the causes of OA, you are empowered to make informed decisions about your health and take a proactive approach to joint care.
Recognizing the Symptoms and Stages
Recognizing the signs of osteoarthritis (OA) early is crucial for effective management. Symptoms often start subtly and progress slowly over time, making it easy to dismiss them at first. However, understanding the key indicators can help you seek treatment sooner.
The Most Common Symptoms of OA
-
Pain: The most prevalent symptom is a deep ache in the affected joint that worsens with activity and improves with rest. It can flare up after periods of inactivity, like when you first wake up in the morning
-
Stiffness: A feeling of stiffness, especially after resting or upon waking, is a hallmark of OA. It typically lasts for a short period (less than 30 minutes) and eases with movement.
-
Swelling: The joint may feel tender to the touch and appear swollen, particularly after a long period of use.
-
Grinding or Popping Sensations: You might hear or feel a clicking, cracking, or grinding sound, known as crepitus, as you move the affected joint. This is caused by the rough surfaces of the bones rubbing together.
-
Loss of Flexibility: As the disease progresses, your range of motion may decrease, making it difficult to fully bend or straighten the joint.
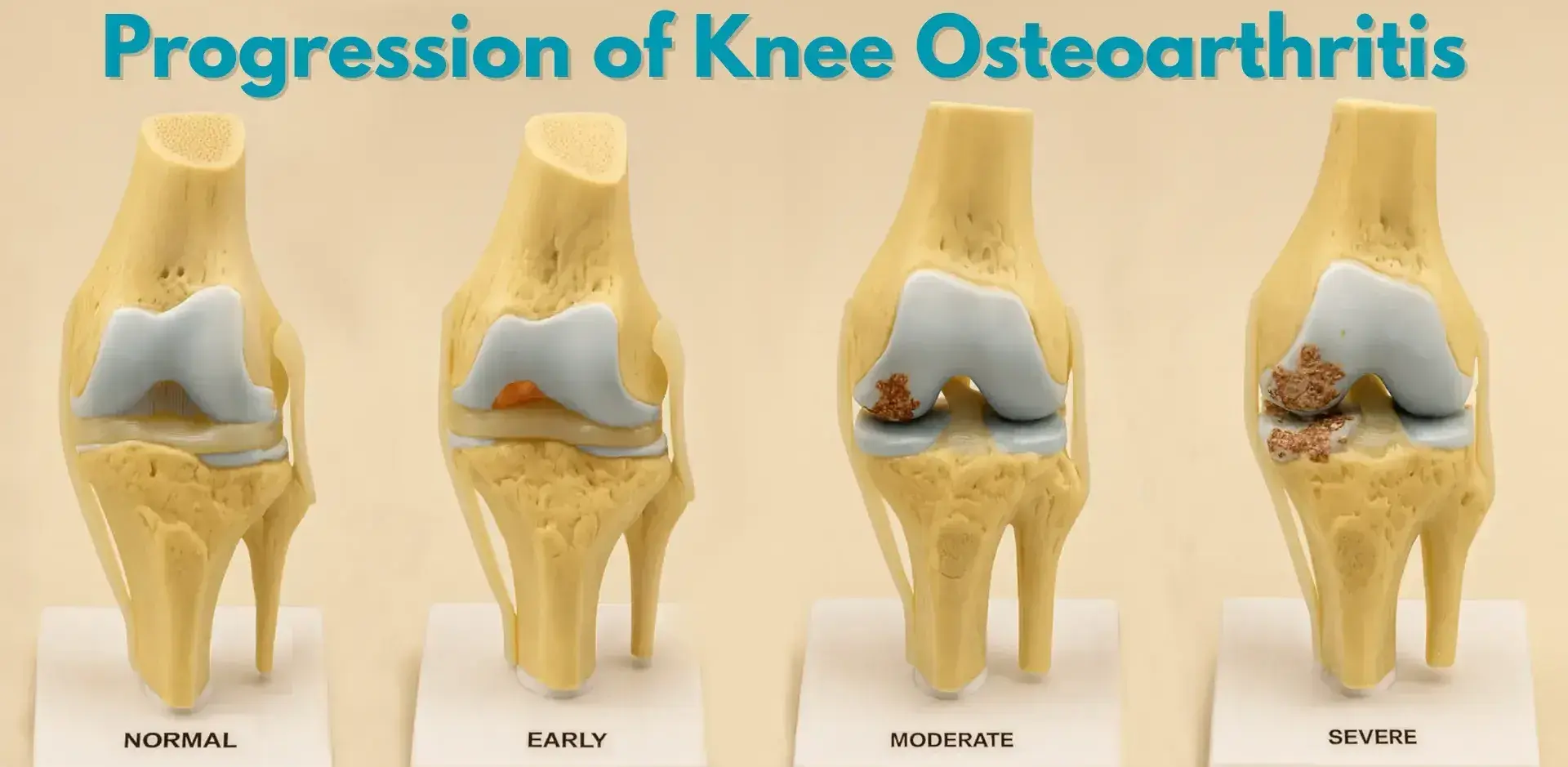
The Four Stages of Osteoarthritis

A healthcare professional will classify the progression of OA into one of four stages, based on the severity of cartilage damage and joint changes observed on an X-ray.
-
Stage 1 (Minor): Very little pain, with only slight cartilage wear visible on X-ray.
-
Stage 2 (Mild): Occasional stiffness and pain after activity. X-ray shows noticeable narrowing of the joint space.
-
Stage 3 (Moderate): Symptoms are more frequent. X-rays reveal significant cartilage damage and clear narrowing of the joint space.
-
Stage 4 (Severe): The most advanced stage. Cartilage is severely worn, leading to bone-on-bone friction and chronic pain.
The Importance of Early Diagnosis
Understanding these symptoms and stages is crucial because early diagnosis can slow the progression of the disease and significantly improve your quality of life. The earlier you seek a professional opinion, the more effective non-surgical treatments like physical therapy and medication can be.
For a deeper dive into how a doctor determines the severity of your condition, read our post, "A Doctor's Guide to Osteoarthritis Diagnosis".
The Diagnostic Process

Getting an accurate diagnosis is the critical first step toward effective osteoarthritis management. A medical professional will use a combination of methods to determine if you have OA and to assess its severity.
Physical Examination
Your doctor will begin with a thorough physical examination of your affected joint. They will check for several key indicators, including:
-
Tenderness: The doctor will gently press on the joint to identify areas of pain.
-
Swelling: They will look for any visible or palpable swelling, which is a common sign of inflammation in the joint.
-
Range of Motion: They will move your joint in different directions to see if it has a reduced range of motion, a hallmark of OA.
-
Sounds: They may listen for grinding or cracking sounds (crepitus) when the joint moves, which can indicate bone-on-bone friction.
X-rays
X-rays are the most important and common tool used to diagnose osteoarthritis. This imaging technique allows doctors to see the state of the bones and the joint space. An X-ray can reveal two key signs of OA:
-
Narrowing of the Joint Space: As cartilage wears away, the space between the bones in the joint decreases. An X-ray can show this narrowing, indicating the extent of cartilage loss.
-
Bone Spurs (Osteophytes): These small, bony growths can form on the edges of the bones as the joint attempts to compensate for the lost cartilage.
X-rays are also used to stage the severity of the disease and monitor its progression over time.
Magnetic Resonance Imaging (MRI)
While X-rays are usually sufficient for a diagnosis, a doctor may order an MRI in certain situations. An MRI provides a detailed look at the soft tissues, including:
-
Cartilage: An MRI can show the condition of the cartilage itself, which may not be visible on a standard X-ray.
-
Ligaments and Tendons: It can also identify damage to ligaments and tendons, which may be contributing to joint instability and pain.
-
Fluid and Inflammation: An MRI can help the doctor see if there is any fluid buildup or inflammation within the joint.
An MRI is particularly useful if a doctor suspects that the pain may be caused by something other than or in addition to OA, such as a meniscus tear.
Once the diagnostic process is complete, your healthcare provider will have a clear picture of your condition, allowing you to discuss a full range of treatment options.
This overview covers the standard imaging, but specialists use specific physical tests to rule out other injuries. To learn exactly what happens during these exams, read our detailed post: A Doctor's Guide to Osteoarthritis Diagnosis.
Non-Surgical Treatment Options for Osteoarthritis
Managing osteoarthritis (OA) often begins with non-surgical treatments aimed at reducing pain, improving joint function, and slowing the progression of the disease. These methods are typically the first line of defense, especially in the early stages of OA.
Lifestyle and Exercise
Making changes to your daily habits can have a significant impact on managing OA symptoms.
-
Weight Management: Reducing body weight is one of the most effective ways to lessen the stress on weight-bearing joints like the knees and hips. Even a small amount of weight loss can lead to a notable decrease in pain and improve joint function.
-
Physical Therapy: A physical therapist can create a personalized exercise program to strengthen the muscles around the affected joint, which provides better support and stability. They can also teach you proper body mechanics to reduce stress during daily activities.
-
Low-Impact Exercise: Activities such as swimming, cycling, and walking put less stress on your joints compared to high-impact exercises like running. These activities are excellent for maintaining mobility and a healthy weight.
Medication and Injections
These treatments focus on managing pain and reducing inflammation.
-
Over-the-Counter Pain Relievers: Medications like ibuprofen (Advil, Motrin) and naproxen sodium (Aleve) can help reduce both pain and inflammation. Acetaminophen (Tylenol) can be effective for pain but does not reduce inflammation.
-
Prescription Medications: If over-the-counter options are not enough, a doctor may prescribe stronger anti-inflammatory drugs or pain relievers.
-
Topical Treatments: Creams, gels, and patches containing pain-relieving ingredients can be applied directly to the affected joint.
-
Corticosteroid Injections: These powerful anti-inflammatory medications are injected directly into the joint. They can provide significant, but temporary, pain relief.
-
Hyaluronic Acid Injections: Hyaluronic acid is a natural component of joint fluid. Injecting it into the joint can improve lubrication and act as a shock absorber, providing some pain relief for certain patients.
Assistive Devices and Supportive Care
In addition to exercise and medication, other measures can help manage symptoms and support your joints.
-
Braces or Wraps: Braces, shoe inserts, or compression wraps can provide support to the joint, help with alignment, and reduce pain during movement.
-
Assistive Devices: Using a cane or a walker can take pressure off painful joints, helping you to remain mobile.
-
Heat and Cold Therapy: Applying heat packs can help relax muscles and increase blood flow, while cold packs can numb the area and reduce swelling after physical activity.
For a full list of actionable tips, read our guide on 10 At-Home Remedies and Exercises for Knee Pain.
Surgical Treatment Options for Osteoarthritis
When non-surgical methods no longer provide sufficient relief, surgical intervention may be considered to restore function and alleviate pain. The choice of surgery depends on a variety of factors, including the severity of the osteoarthritis, the patient's age, and their activity level.
Total Joint Replacement (TJR)
Total joint replacement is a proven and highly effective solution for severe, end-stage osteoarthritis. The procedure involves removing the damaged cartilage and bone and replacing them with a new joint made of metal, plastic, or ceramic. The most common types are total knee replacement and total hip replacement. TJR can provide dramatic pain relief and restore mobility, allowing many patients to return to an active lifestyle.
Osteotomy
An osteotomy is a surgical procedure that involves cutting and reshaping the bone to realign the joint and shift the weight from the damaged part of the joint to a healthier area. It is typically performed on younger, more active patients with early-stage osteoarthritis. The goal is to delay the need for a total joint replacement by preserving the patient's natural joint for as long as possible.
Arthroscopic Joint Resurfacing
Arthroscopic joint resurfacing is a minimally invasive procedure designed to treat localized cartilage damage. Instead of replacing the entire joint, a surgeon uses a small camera (arthroscope) to repair or replace only the damaged area of the joint. This approach offers several benefits, including a smaller incision, less blood loss, and a potentially faster recovery time compared to a total joint replacement. This method is particularly suitable for patients with focal cartilage defects rather than widespread joint degeneration.
The decision to pursue surgery should be made in consultation with an orthopedic surgeon, who can discuss the risks, benefits, and expected outcomes of each procedure. The right choice of treatment is one that is tailored to your unique condition and lifestyle.
Formae CyborGel®: A Potential Solution for Joint Preservation & Treatment of OA
While total joint replacement is a proven solution for severe osteoarthritis, it is a major surgery that can be avoided in many cases. At Formae, our mission is to engineer innovative solutions that preserve the joint and help people return to an active, pain-free life without the need for an invasive total replacement.
Our product, CyborGel®, is a synthetic biomimetic cartilage implant designed for arthroscopic joint resurfacing. Unlike traditional treatments that replace the entire joint or offer only temporary pain relief, CyborGel® is designed to address the specific, localized cartilage damage that is common in early to mid-stage osteoarthritis.
How It Works
CyborGel® is a small, bio-synthetic GelPlug that is engineered to be implanted into the areas of the joint where cartilage has worn away. Its unique composition is designed to mimic the properties of natural cartilage, providing a smooth, durable, and lubricious surface that allows the joint to function without the painful bone-on-bone friction. The implant is designed to be highly durable, allowing it to withstand millions of cycles without progressive wear.
Key Advantages
-
Minimally Invasive: The procedure to implant CyborGel® is performed arthroscopically, using small incisions. This can lead to less blood loss, less post-operative pain, and a faster recovery time compared to open surgery.
-
Joint Preservation: CyborGel® treats only the damaged area of the joint, leaving the healthy parts of the knee intact. This is a significant advantage over total joint replacement, which involves removing the entire joint.
-
Durable and Effective: The biomimetic properties of the implant are designed to provide long-lasting pain relief and restore natural joint function.
CyborGel® is a potential solution for patients with focal cartilage defects who are looking for a less-invasive alternative to total joint replacement. By choosing joint preservation, you can take a proactive step toward maintaining your mobility and quality of life.
Summary
Osteoarthritis is a complex and progressive joint disease, but it is not an inevitable part of aging. From lifestyle modifications and physical therapy to cutting-edge surgical solutions like arthroscopic joint resurfacing, a wide range of effective treatments are available. By understanding the causes, recognizing the symptoms early, and exploring all your options, you can take control of your condition and reclaim your mobility.
The journey to an active, pain-free life begins with making an informed decision about your joint health. At Formae, we are dedicated to providing innovative solutions that bridge the gap between conservative treatments and invasive total joint replacement.
